Oral Surgery
What Are Wisdom Teeth?
Third molars are commonly referred to as wisdom teeth. They are usually the last teeth to develop and are located in the back of your mouth, behind your second molars. Their development is usually completed between the middle teenage years and early twenties, a time traditionally associated with the onset of maturity and the attainment of wisdom.
Types Of Impactions:
We will need to see you for a consultation to determine if you will benefit from wisdom tooth removal. A special x-ray of your mouth and jaws (panorex) will be taken to determine if your wisdom teeth are impacted, if there is room for them to erupt, and how difficult it will be to have them removed
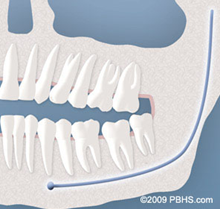
- Soft Tissue Impaction: There is not enough room to allow the gum tissue to retract for adequate cleaning of the tooth.
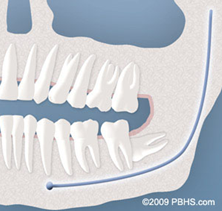
- Partial Bony Impaction: There is enough space to allow the wisdom tooth to partially erupt. However, the tooth cannot function properly in the chewing process, and creates cleaning problems, among others.
- Complete Bony Impaction: There is NO space for the tooth to erupt. It remains embedded in the jaw bone or if even partially visible requires complex surgical techniques for removal.The impacted wisdom tooth may also be in an unusual position and difficult to remove. This situation can also arise when the shape or size of the jaw bone and other facial structures make removal of this tooth significantly more complex.
Soft Tissue
Partial Bony

Complete Bony

Complete Bony
TMJ Disorders and Facial Pain
We believe in using evidence-based medicine to help our patients make real and positive improvements. The practice employs a caring, committed approach that is individualized for each and every patient. Our team are passionate about the pursuit of excellence in the treatment of temporomandibular disorders and are constantly learning so as to provide the highest quality and effectiveness of treatment for every patient..
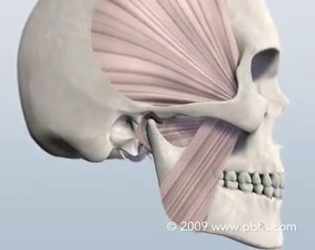
WHAT IS TMD/TMJ?
TMD stands for temporomandibular disorders and encompasses a range of facial pain/dysfunction conditions that include intra-articular (inside the joint) and muscular problems. One of the major problems with TMD is that there is still no consensus on the cause, how to prevent, or how to treat these disorders. Fortunately though, if we pay heed to the quality scientific evidence that is available to us, we can treat these problems successfully. For most patients, the problem is nothing more than a strained/sprained joint. While most practitioners view TMD as a predominantly dental problem, the truth is that the TMJ is a joint, much like an ankle, a knee or a shoulder and should be diagnosed and treated as such. For patients with acute injuries, resting the joint and performing simple, conservative treatment will resolve the problem in a short period of time. For others the problem is chronic and requires more advanced treatment modalities. Because the TMJ complex is made up of living bone, ligaments and muscles, it is capable of repair, adaptation and healing.
WHAT ARE THE SYMPTOMS?
- Pain in front of the ears (during opening, closing, chewing)
- Clicking, popping, grinding, swooshing noises in the joints
- Jaw locking closed or open
- Pain or fatigue in the chewing muscles
- Headaches
- Earaches
- Tinnitus (ringing in the ears)
- Changes in occlusion (teeth not hitting correctly)
Treatment
Treatment varies and may be different for each patient. Your treatment plan and care will be customized and tailored to your specific needs and diagnosis. Treatment options range from simple self-care to custom total joint replacement. Because, for most patients, TMD symptoms are usually self-limiting, simple, conservative modalities are used as first line treatments.
It is important to understand that TMD is a musculoskeletal disorder as opposed to a dental disorder and the teeth have little to do with it. Part of your initial appointment will involve your doctor formulating a special, individualized treatment plan that is tailor-made just for you..
Snoring and Sleep Apnea
People with obstructive sleep apnea (OSA) have disrupted sleep patterns associated with airway obstruction resulting in low blood oxygen levels as well as cardiovascular disease. When obstructive sleep apnea occurs, the airway is obstructed by excess tissues in the throat or tongue. This blocks the upper airway reducing or completely obstructing airflow. When the oxygen level in the brain becomes low enough, the sleeper partially awakens, the obstruction in the throat clears and the flow of air starts again, usually with a loud gasp.
Repeated cycles of decreased oxygenation lead to very serious cardiovascular problems. Additionally, these individuals suffer from excessive daytime sleepiness, depression, and loss of concentration.
Some patients have obstructions that are less severe called Upper Airway Resistance Syndrome (UARS). In either case, the individuals suffer many of the same symptoms.
The first step in treatment resides in recognition of the symptoms and seeking appropriate consultation.Oral and maxillofacial surgeons offer consultation and treatment options.



